CAA Comment
This is another insightful article in this important series, dealing with the inevitable pushback from the pro-drug injecting room lobby.
What is not addressed is the weight that should be given to this group and do they have a vested interest.
The argument is over establishing Homelessness and Addiction Recovery Treatment (HART) Hubs in lieu of safe injecting rooms.
A very similar concept to the position of the CAA.
As a society, we would not tolerate accepting that a person with any sort of health issue was not treated, but rather, their affliction or disease was just managed, and the causes were actively facilitated when cures were available.
We will be closely watching the legal ramifications of the options to close and modify Injecting Rooms and convert them to Hart Hubs. Altogether a sound strategy from which addicts may recover from their illness rather than the addiction being fed.

The operator of a Toronto overdose prevention site is challenging Ontario’s decision to prohibit 10 supervised consumption sites from offering their services.
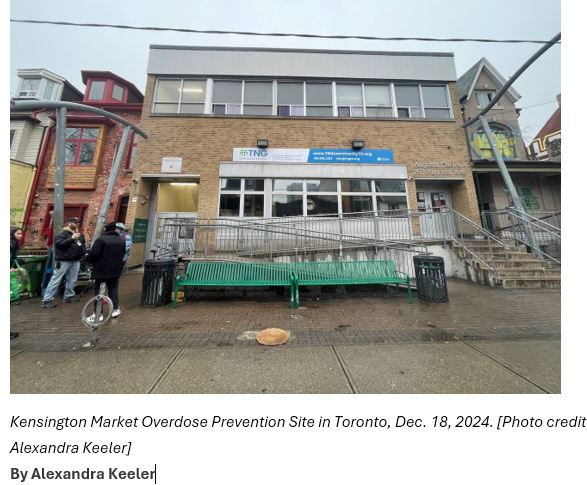
In December, Neighbourhood Group Community Services and two individuals launched a constitutional challenge to Ontario legislation that imposes 200-metre buffer zones between supervised consumption sites and schools and daycares. The Neighbourhood Group will be forced to close its site in Toronto’s Kensington Market as a result.
In its court challenge, the organization is arguing site closures discriminate against individuals with “substance use disabilities” and increase drug users’ risk of death and disease.
The challenge is the latest sign of growing opposition to Ontario’s decision to either shutter supervised consumption sites or transition them into Homelessness and Addiction Recovery Treatment (HART) Hubs. The hubs will offer drug users a range of primary care and housing solutions, but not supervised consumption, needle exchanges or the “safe supply” of prescription drugs.
Critics say the decision to suspend supervised consumption services will harm drug users and the health-care system.
“We’re very happy that the HART Hubs are being funded,” said Bill Sinclair, CEO of Neighbourhood Group Community Services. “They’re a great asset to the community.”
“[But] we want HART Hubs and we want supervised consumption sites.”
‘Come under fire’
On Thursday, the Ontario government announced that nine of the 10 supervised consumption sites located near centres with children would transition into HART Hubs. The Neighbourhood Group’s site is the only one not offered the opportunity to transition, because it is not provincially funded.
Laila Bellony, a harm reduction manager at a supervised consumption site at the Parkdale Queen West Community Health Centre in Toronto, says she is worried that drug users may avoid using HART Hubs altogether if they do not facilitate the use of drugs under the supervision of trained staff.
Data show this oversight can prevent deaths by facilitating immediate intervention in the event of an overdose.
Bellony is also concerned the site closures will increase the strain on other health-care services. She predicts longer wait times and bed shortages in hospital emergency rooms, as well as increased paramedic response times.
“I think the next thing that will happen is the medical or health-care system is going to come under fire for being sub-par. But it’s really all starting here from this decision,” she said.
She questions how the HART Hubs will meet demand for detox and recovery services or housing solutions.
Parkdale Queen West Community Health Centre and its sister site, the Queen West Site, serve hundreds of clients, Bellony says. By contrast, Ontario’s HART Hub rollout plan indicates all 19 hubs will together provide 375 new housing units across the province.
“The HART Hub model is not a horrible model,” said Bellony. “It’s the way that it’s being implemented that’s ill-informed.”
In a response to requests for comment, a media spokesperson for the Ontario Ministry of Health directed Canadian Affairs to its August news release. That release lists proposals for increased safety measures at remaining sites, and a link to a HART Hub “client journey.”
On Dec. 3, the Auditor General of Ontario, Shelley Spence, released a report criticizing the health ministry’s “outdated” opioid strategy, noting it has not been updated since 2016.
National data show a 6.7 per cent drop in opioid deaths in early 2024. But experts caution it is too soon to call it a lasting trend. Opioid toxicity deaths in 2023 were up 205 per cent from 2016.
“We concluded that the Ministry does not have effective processes in place to meet the challenging and changing nature of the opioid crisis in Ontario,” the auditor general’s report says.
“The Ministry did not … provide a thorough, evidence-based business case analysis for the 2024 new model … [HART Hubs] to ensure that they are responsive to the needs of Ontarians.”
 ‘Ill-informed’
‘Ill-informed’
Ontario has cited crime and public safety concerns as reasons for blocking supervised consumption sites near centres with children from offering their services.
“In Toronto, reports of assault in 2023 are 113 per cent higher and robbery is 97 per cent higher in neighbourhoods near these sites compared to the rest of the city,” Ontario Health Minister Sylvia Jones’ office said in an Aug. 20 press release.
The province has also cited concerns about prescription drugs dispensed through safer supply programs being diverted to the black market.
Police chiefs and sergeants in the Ontario cities of London and Ottawa have confirmed safer supply diversion is occurring in their municipalities.
“We are seeing significant increases in the availability of the diverted Dilaudid eight-milligram tablets, which are often prescribed as part of the safe supply initiatives,” London Police Chief Thai Truong said at a Nov. 26 parliamentary committee meeting examining the effect of the opioid epidemic and strategies to address it.
But Bellony disputes the claim that neighbourhoods with supervised consumption sites experience higher crime rates.
“Some of the things that [the ministry is] saying in terms of crime being up in neighbourhoods with safe consumption sites — that’s not necessarily true,” she said.
In response to requests for information about the city’s crime rates, Nadine Ramadan, a senior communications advisor for the Toronto Police Service, directed Canadian Affairs to the service’s crime rate portal.
The portal shows assaults, break-and-enters and robberies in the West Queen West neighbourhood have remained relatively stable since the Queen West supervised consumption site opened in 2018.
In contrast, crime rates are higher in some nearby neighbourhoods without supervised consumption sites, such as The Junction.
“While I can’t speak to perceptions about a rise in crime specifically around supervised consumption sites, I can tell you that violent crime is increasing across the GTA,” Ramadan told Canadian Affairs. She referred questions about Jones’ statements about crime data to the health minister’s office.
Jones’ office did not respond to multiple follow-up inquiries.
Mixed feelings
In July, Canadian Affairs reported that business owners in the West Queen West neighbourhood were grappling with a surge in drug-related crime.
Rob Sysak, executive director of the West Queen West Business Improvement Association, says there are mixed feelings about their neighbourhood’s site ceasing to offer safe consumption services.
“I’m not saying [the closure] is a positive or negative decision because we won’t know until after a while,” said Sysak, whose association works to promote business in the area.
Sysak says he has heard concerns from business owners that needles previously used by individuals at the site may now end up on the street.
Bellony supports the concept of HART Hubs, offering addiction and support services. But she says she finds the province’s plan for the hubs to be unclear and unrealistic.
“It seems very much like they kind of skipped forward to the ideal situation at the end,” she said. “But all the steps that it takes to get there … are unaddressed.”